If you’ve been following the news out of Washington DC over the past week, you know it’s been a complete fracas within the House of Representatives on the Republican side of the aisle. Here’s what went down, and how it relates to health care issues and bills.
Continuing Resolutions vs. Government Shutdown
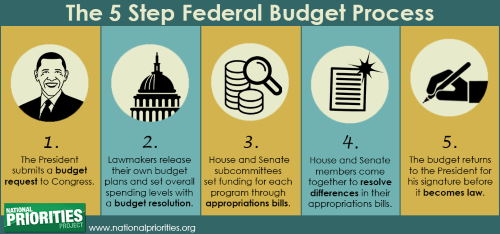
Late last week, House Republicans serially put forward two “Continuing Resolution” (CR) proposals to keep the federal government temporarily funded, open, and operating. The larger backdrop for this situation is the failure of Congress to enact 12 appropriations bills that comprise the annual federal budget before the start of the new federal fiscal year on October 1st. Theoretically, this year these bills are supposed to conform to a broad budget outline laid out in the Fiscal Reduction Act (FRA) that was enacted last spring to avert the federal government from defaulting on its debt.
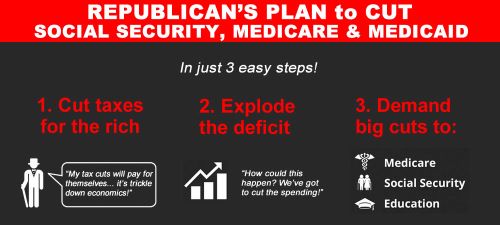
The first CR (HR 5525) taken up Friday afternoon (Sept. 29) reflected the demands of many conservative Republicans, in violation of the FRA deal. It contained large spending cuts to “discretionary” social programs, spending increases for national defense and homeland security, creation of a special commission to cut spending for “mandatory programs” (i.e., Social Security, Medicare, Medicaid), and a host of non-budget “hot button” social issues (like restrictions on reproductive freedom for women and health care for transgender people.) Here’s a good summary of what was in this first CR and its predicted impacts.
This CR failed to pass the House because the spending cuts weren’t deep enough for a small number far-right Republicans, so they voted against it. The Democratic Minority opposed it because of the spending cuts, the special commission idea, and the social issue riders. All NY Republicans voted for this CR, and all NY Democrats against.
A second CR (HR 5860) taken up Saturday afternoon (Sept. 30) reflected a bipartisan consensus that has been emerging over in the Senate. It was a “clean” CR that just kept the current FY 2023 federal budget in place with no spending cuts or special commission or extraneous social issue riders. There was also a bit of new special spending to help states and localities respond to recent natural disasters (floods, hurricanes, tornadoes, wildfires, etc.) All Democrats (but one) joined with slightly more than one-half of the Republicans to pass this new CR, and it then was sent over and passed by the Senate and then signed by President Biden. All Reps. from New York (both Republicans and Democrats) voted for it.
Political sideshow: This result triggered a revolt among a small group of far-right Republicans in the House such that they undertook a successful effort to remove House Speaker McCarthy earlier this week. Now the House is unable to undertake any legislative business until a new Speaker is chosen. An interim speaker is in place to oversee that process, Rep. Patrick McHenry (R-NC).
Appropriations Bills for a FY 2024 Federal Budget
Meanwhile, the process to adopt an annual budget for FY 2024 resumes as House committees continue their work to finalize their ideas for various appropriations bills – the Senate has completed the committee process on a bipartisan basis. We health care advocates will be paying attention to the “Labor-HHS” appropriations bills that cover all things health care. We’ll also be focusing on renewed funding for community health centers and safety net hospitals.
The new deadline for enactment of all these appropriations bills in agreement with the Senate and White House is now Fri. Nov. 17, in order to avert a government shutdown. It’s also possible that another CR process may have to take place then.
Our basic message to Congress remains: “Stick to the bipartisan agreement enacted last spring under the Fiscal Responsibility Act as you finish up the appropriations bills. Any special commission proposal and social issue riders should be set aside during this budget process, and debated separately at another time.
Stand-Alone Health Care Bills
1. Health care costs and transparency — Since the beginning of this year, committees in both the Senate and House have been crafting modest, bipartisan bills to a) regulate “pharmacy benefit managers” (PBMs), and b) improve transparency with regard to health care prices, particularly hospital-based services.
On the House side of things, various bills have been packaged together into the “Lower Costs, More Transparency Act” (HR 5378) – here’s a summary of the bill’s provisions. No members of New York’s House delegation –either Republicans or Democrats– are yet on this bill as co-sponsors.
On the Senate side, we await a package that will combine proposals from the Finance Committee, and the Health, Education, Labor, and Pensions Committee. It is expected to come forward later this fall once the budget process is done. Once it is out, negotiations will commence between the House and Senate and White House to come to agreement on a final bill that may pass by the end of this calendar year.
2. Rx drugs – The historic Inflation Reduction Act (IRA) is taking on the pharmaceutical industry in various ways to rein-in its long-running and widespread price-gouging and profiteering practices. However, this new law’s scope is limited to Medicare. The “Lower Drug Costs for American Families Act” (HR 4895) will build out the IRA’s Rx drug provisions beyond Medicare to other kinds of health insurance – here’s a summary.
So far, only 5 House Reps. from NY are co-sponsoring this bill: Goldman, Meng, Morelle, Nadler, and Tonko. It’s important to reach out to the rest of the delegation about it, to build momentum. No companion bill has yet been introduced in the Senate, but one is in development and expected out later this fall.
It’s important to note that public opinion research shows that support for taking on Big Pharma to lower drug prices and costs for patients is exceptionally high across the political spectrum, so this bill is a slam-dunk winning issue for us to push forward.
3. Reproductive Freedom – The Women’s Health Protection Act (S.701/Baldwin, HR 12/Chu) would create a national law to guarantee the right to provide and access abortion care. Here is a bill summary. New York co-sponsors include Senators Schumer and Gillibrand, and all Democratic Reps. (Bowman, Clarke, Espaillat, Goldman, Higgins, Jeffries, Meeks, Meng, Morelle, Nadler, Ocasio-Cortez, Ryan, Tonko, Torres, Velazquez.)
4. Universal Health Care — Finally, we want to remind everyone that Medicare-for-All bills were introduced this past spring in each chamber, a goal we have supported for three decades now. These bills would create a truly universal health care program covering all Americans, and they have significant numbers of co-sponsors. HR 3421/Jayapal-Dingell has 112 co-sponsors, including 12 from NY (Bowman, Clarke, Espaillat, Goldman, Higgins, Meeks, Meng, Nadler, Ocasio-Cortez, Tonko, Torres, and Velazquez), S.1665/Sanders has 14 co-sponsors including Sen. Gillibrand from NY. Sen. Schumer supports it too, but given his position as Majority Leader he typically does not co-sponsor bills.
Given the current political constellation of Congress, neither of these two latter bills are expected to move forward at present. However, they are important “goal bills” to point to as we focus also on those bills that are moving ahead. For us, our advocacy is never an either-or matter, but always a both-and one. We know it’s essential to focus on both longer-term and immediate matters to be most effective, and that a crucial political synergy exists between them – each effort enhances the other.
We urge everyone to reach out to your own member of Congress about any or all of the above matters, as well as Senators Schumer and Gillibrand.